BIOLOGICAL ACTION OF HORMONES
1. Glucocorticoids: structure of cortisol, target tissues, effects on metabolism and functions.
Hyper- and hypoproduction of the hormones.
2. Mineralocorticoids: structure of aldosterone, target tissues, biological effects. Hyper- and
hypoproduction of the hormones.
3. Female sex hormones: structure of estradiol and progesterone, target tissues, effects on
metabolism and functions. Hyper- and hypoproduction of the hormones.
4. Male sex hormones: structure of testosterone, target tissues, effects on metabolism and
functions. Hyper- and hypoproduction of the hormones.
5. Hormones of hypothalamus and hypophysis, their biological action. Growth hormone,
adrenocorticotropic hormone: target tissues, effects on metabolism. Hyper- and
hypoproduction of growth hormone.
6. Eicosanoids (prostaglandins, thromboxanes, leukotrienes) and their role in the regulation
of metabolism and functions.
7. Disorders of functions of endocrine glands: hyper- and hypoproduction of hormones.
ADRENAL CORTEX produces steroid hormones:
1. Glucocorticoids
2. Mineralocorticoids
3. Male and female sex hormones.
1. Glucocorticoids: structure of cortisol, target
tissues, effects on metabolism and functions.
Hyper- and hypoproduction of the hormones.
01. Glucocorticoids
(GCs): cortisol, cortisone and
corticosterone.
Structure of
cortisol
Target-tissues for
GCs:
1. Liver
2. Muscle
3. Adipose
4. Connective
5. lymphoid
tissues
• In
the liver, GCs ↑ anabolic processes
and ↑ transport of substrates into the cell (↑ permeability of membranes), and
metabolism GCs can influence:
• Асtion of
glucocorticoids
1. on
METABOLISM
2. SYSTEMIC action
1) Carbohydrate
metabolism
2) Lipid
metabolism
3) Protein
and amino acid metabolism
The effects of GCs on metabolism
01. Carbohydrate metabolism.
GCs ↓ glycolysis in all the target-tissues.
• In
the liver, GCs ↑ gluconeogenesis and
synthesis of glycogen.
• In
the other tissues, GCs ↓ transport
of glucose into the cell (↓ permeability of membranes).
The excess
of GCs ↑ the blood glucose level and may cause steroid diabetes.
02. Lipid metabolism.
• In
the liver, GCs ↑ synthesis of fats
(triacylglycerols), VLDL, and ketone bodies.
• In
the adipose tissue GCs ↑ degradation
of triacylglycerols on the extremities but ↑ deposition of the triacylglycerols
on the trunk and on the face.
The excess of GCs causes the spider-like obesity, and ↑ [ketone
bodies] in the blood.
03. Protein and amino acid metabolism.
• In
the liver, GCs ↑ synthesis of
protein and ↓ its degradation.
• In
the other target-tissues, GCs ↓
synthesis of protein, ↑ its degradation.
The excess of GCs leads to:
-
muscle atrophy and weakness;
-
the decrease of collagen synthesis → bone
fragility and fractures at minimal trauma; slowdown of wounds’ healing;
-
in the lymphoid tissue GCs decrease synthesis of antibodies, lymphocyte formation and cause
destruction of these cells
• ↑
susceptibility to infections.
• used
for treatment of some allergic reactions
• GCs
are used in transplantation of organs because they suppress the immune response
Systemic effects of GCs:
1) ↑
secretion of HCl in the stomach (GCs ↓ synthesis of prostaglandins which ↓
secretion of HCl). The excess of GCs may cause stomach ulcers.
2) GCs have anti-inflammatory
effect and may be used for treatment of inflammation. (GCs ↓ synthesis of
prostaglandins – tissue inflammatory factors).
3) ↓
hypersensitivity of the organism, and may be used for treatment of allergy
(e.g. anaphylactic shock).
2. Mineralocorticoids: structure of aldosterone,
target tissues, biological effects. Hyper- and
hypoproduction of the hormones.
Aldosterone and dehydroxycorticosterone regulate metabolism of Na+, K+ and water in the
organism.
Structure of aldosterone
The target-tissue:
epithelial cells of the distal renal
tubules.
Aldosterone is called sodium-retaining hormone because in the
kidney it ↑ reabsorption of Na+ from the
urine and ↑ [Na+].
Water follows the flow of Na+ → → the ↑ of
the circulating blood volume.
The excess of aldosterone → → the ↑ BP and edema (swelling of tissues).
The sodium reabsorption increases the potassium excretion in urine.
Aldosterone ↑ excretion of K+ into the urine.
The excess of aldosterone leads to the ↓
of [K+] in the blood → → heartbeat
impairments, heart failure, and heavy weakness.
Sweat glands
are another target-tissue for aldosterone.
The heat (high outer temperature) stimulates
aldosterone production due to which the excessive
sodium loss via the sweat is prevented.
Deficiency of aldosterone in the organism
results in the loss of sodium and water
with the urine and dehydration of the body.
Glucocorticoids, especially corticosterone, exert
partial mineralocorticoid effects on the organism; therefore in the use of
glucocorticoids as therapeutic agents, the potassiumcontaining medicines should
be prescribed to the patient.
Hypercorticoidism 3 types:
1. Glucocorticoid
excess (hyperfunction of zona
fasciculata of adrenal cortex) Cushing’s syndrome (malignant adrenal cortex
tumor) Cushing’s disease (benign
enlargement of the adrenal glands).
2. Mineralocorticoid
excess (hyperfunction of zona
arcuata) - Konn’s disease.
3. Adrenal
virilism, or adrenogenital syndrome (hyperproduction of male sex
hormones in zona reticulata of adrenal cortex).
In females, this leads to virilism (appearance of
male signs);
in males, the ↑ of male signs; in children –
premature sex developing (maturation before puberty).
Hypocorticoidism (Addison’s disease or bronze
disease)
This is hypofunction of the adrenal
cortex, ↓ both mineralocorticoids and glucocorticoids.
Symptoms:
bronze pigmentation of the skin, weakness, hypoglycemia (hunger intolerance),
subconscious preference of salt meals, the ↓ BP.
3. Female sex hormones: structure of estradiol and
progesterone, target tissues, effects on
metabolism and functions. Hyper- and hypoproduction of the hormones.
01. ESTROGENS
- estradiol (is formed in ovaries),
- estriol (in placenta),
- (in adrenal cortex),
The target-tissues
and effects:
• sex
organs – development and functioning of sex organs;
• non-sex
organs:
1) CNS:
formation of sexual behaviour, instinct, and psychical status of a female.
2) Bones,
larynx: formation of the female type of the skeleton, larynx and voice.
Estrogens ↑ ossification of epiphyses
where the growth zone of the bone is located.
In a girl, lack of estrogens may cause tall height.
In women, excess of estrogens ↑ deposition of Ca in the bone cavities where the red
bone marrow is located; therefore anemia
may take place.
3) Skin
– ↑ growth of hair on the female type, ↓ hair growth on the trunk and face, ↓
secretory activity of the sebaceous glands.
4) Adipose tissue
– ↑ synthesis of triacylglycerols, promote formation of the typically female
fat depositions.
5) Kidney
–
In pregnancy (much progesterone) the loss of Na+ with the urine explains the subconscious preference of the salt food.
6) Liver. Estrogens ↑ synthesis of:
a) blood
clotting factors (II, VII, IX, X) and angiotensinogen; excess of estrogens
may cause thromboses and hypertension
(↑BP).
b) VLDL and
HDL; VLDL transfer triacylglycerols from the liver to adipose tissue,
therefore, in female, muscles are always covered by the layer of subcutaneous
adipose tissue.
HDL remove
cholesterol off the organism; therefore atherosclerosis and myocardial
infarction (as consequences of the increased cholesterol level in the blood)
are more often observed in men than in women.
4. Male sex hormones: structure of testosterone,
target tissues, effects on metabolism and
functions. Hyper- and hypoproduction of the hormones.
MALE SEX HORMONES (androgens):
testosterone and androsterone. They are formed in
1. testes,
2. adrenal
cortex,
3. prostate
gland.
They are also formed in ovaries
Androgens are inactivated in the liver with the
resultant formation of 17-ketosteroids which are excreted into the urine.
Androgens exert generalized anabolic effect on the
organism:they stimulate synthesis of nucleic acids and proteins, retain
nitrogen and calcium in the organism, and increase synthesis of the membrane
phospholipids.
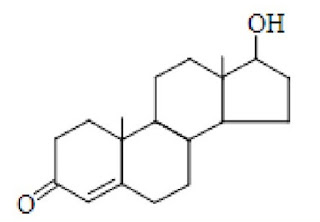
Structure of testosterone
The
target-tissues and effects:
• sex
organs – the hormones exert androgenic effect (development and functioning of
sex organs).
• non-sex
organs:
1) CNS: formation of sexual behaviour, instinct, and
psychical status of a male. Excess of androgens may cause aggressiveness.
2) Bones, larynx:
formation of the male type of the skeleton, larynx and voice.
Androgens ↑ ossification of epiphyses (the
growth zone of the bone).
The excess of androgens may lead to the short
height.
3) Muscles
– ↑ synthesis of protein in the skeletal muscle, its mass and strength.
4) Adipose tissue
– ↓ synthesis of triacylglycerols and ↑ their degradation; therefore in men the
subcutaneous fat layer is thinner than in women.
5) Skin
– ↑ growth of hair on the male type, stimulate hair growth on the trunk and
face, pigmentation of the skin, secretory activity of the sebaceous
glands.
Excess of androgens may be a reason of baldness (
the absence of hair on the head).
5. Hormones of hypothalamus and hypophysis, their
biological action. Growth hormone, adrenocorticotropic
hormone: target tissues, effects on metabolism. Hyper- and hypoproduction of growth hormone.
THE SYSTEM OF
HYPOTHALAMUS-HYPOPHYSIS IN REGULATION OF ENDOCRINE GLANDS
Synthesis of hormones and their secretion into the
blood are regulated by the requirements of the organism.
Hormones are released into the blood in response to
the appropriate stimulation.
The impulses from receptors reach (via afferent nerves) the CNS, there the impulses are analyzed and then (via efferent
nerves) sent to the periphery.
But the nervous regulation doesn’t cover all functions of all organs; therefore it is
supplemented by hormonal regulation.
The site
of joining the nervous and hormonal regulation is the hypothalamus.
Under the influence of nervous impulses from the
CNS, liberins and statins are
formed in hypothalamus.
Liberins
stimulate and statins inhibit synthesis of tropic hormones of the hypophysis (pituitary gland), i.e. the anterior lobe of hypophysis known as adenohypophysis.
Hormones generated here enter the blood, are
transported to the peripheral endocrine
glands and stimulate production of
definite hormones.
The hormones of adenohypophysis include:
1. Growth hormone (GH; somatotropin) acts
on the bone tissue to accelerate its growth.
2. Thyroid stimulating hormone (TSH)
stimulates growth of the thyroid gland and secretion of thyroxine.
3. Adrenocorticotropic hormone (ACTH)
stimulates growth of the adrenal cortex and increases mainly secretion of
cortisol.
4. Gonadotropic hormones:
follicle-stimulating hormone (FSH),
luteinizing hormone (LH) and prolactin (or lactotropic hormone,
LTH).
They influence development
and the hormone secretion of ovaries in females and testes in males.
Prolactin stimulates lactation.
The posterior lobe of hypophysis called neurohypophysis
contains hormones oxytocin and
vasopressin which are synthesized in supraoptical
and paraventricular nuclei of hypothalamus but are stored in the posterior
lobe of the hypophysis.
1.
Oxytocin
stimulates the uterus to contract during the childbirth and causes production
of milk from the mammary glands.
2.
Vasopressin,
or antidiuretic hormone (ADH)
stimulates reabsorption of water by the kidney tubules and causes
vasoconstriction resulting the increase of the blood pressure. In the posterior
lobe atrophy, diabetes insipidus is
developed (urinary excretion is extremely large, 10-20 liters per day).
Of all hormones produced in the adenohypophysis,
growth hormone and ACTH exert the most expanded biochemical and physiological
effects on the organism.
GROWTH HORMONE, its action
1) Anabolic effect. GH ↑ synthesis of nucleic acids
and proteins in bones, cartilages, and soft tissues.
2) Diabetogenic effect. In the liver, GH ↑
gluconeogenesis.
In the muscle and adipose tissue, GH ↓
membrane permeability for glucose to enter the cell.
Excess of GH leads to the insulinoresistancy of
peripheral tissues and results in somatotropic diabetes.
3) Lipolytic effect. In children, the adipose stores
are absent because in the adipose tissue GH ↑ cleavage of
triacylglycerols.
Due to lipolytic effect and further
utilization of fatty acids, in excess of GH, the ↑ amount of ketone bodies is
produced in the liver and their concentration in the blood ↑.
Hypersecretion of
GH
In childhood, this leads to gigantism: excessive height, the
extremities are disproportionally long.
In adults, this results in acromegaly: intensive
enlargement of individual parts of the skeleton bones (superciliary archs,
cheekbones, jaw and chin), enlargement of the soft tissues of the face (lips,
nose, tongue).
in childhood leads to the proportional underdevelopment of the skeleton and the
whole body.
Unlike in cretinism, no psychic abnormalities and no
skeletal deformations.
ACTH:
target tissues and effects
1)adrenal cortex – ↑ synthesis and secretion of
glucocorticoids and (to less extent) mineralocorticoids;
2)adipose tissue – ↑ cleavage of triacylglycerols;
3) liver – ↑cleavage of glycogen.
6. Eicosanoids (prostaglandins, thromboxanes, leukotrienes)
and their role in the regulation of
metabolism and functions.
PROSTAGLANDINS
AND OTHER EICOSANOIDS
This is a group of local, or tissue hormones, or hormone-like
substances, because unlike “real” hormones that are synthesized in one type of organs but act in the other one,
eicosanoids are both formed and act at the same tissues.
These substances are called eicosanoids because they are
produced from eicosatetraenoic,
or arachidonic,
acid.
Eicosanoids (prostaglandins,
prostacyclins, thromboxanes, and leukotrienes) are synthesized from arachidonic acid (Fig. 14.1.).
-
This polyunsaturated fatty acid is released from
membrane phospholipids by phospholipase
A2.
-
The enzyme is inhibited by glucocorticoids (antiinflammatory agents).
-
Arachidonic acid is
oxidized by cyclooxygenase to form prostaglandins, prostacyclins and
thromboxanes.
-
Cyclooxygenase
is inhibited by aspirin, indomethacin,
and other nonsteroidal antiinflammatory agents.
-
Leukotrienes can
be produced from arachidonic acid by
a pathway in which lipoxygenase
participates; its activity is inhibited by vitamin E, and vitamin P.
Prostacyclins
dilate arteries, ↓ aggregation of platelets.
Thromboxanes
cause vasoconstriction and ↑ aggregation of platelet.
Leukotrienes
take part in inflammation, allergic reactions, and immune response, attract
leucocytes to the place of inflammation, constrict bronchi, and ↑ secretion of
bronchial mucus.
Prostaglandins
are synthesized in all cells excepting erythrocytes, and degraded very quickly
– in 20 minutes.
Major classes of prostaglandins which have clinical
importance:
-
Prostaglandins E
-
Prostaglandins F Prostaglandins E:
1) ↓
cleavage of triacylglycerols and glycogen;
2) are
the tissue inflammatory factors; ↑ permeability of vessels and cell membranes,
dilate capillaries; they are pyrogenic agents, i.e. they ↑ the body t° ;
therefore aspirin (as an inhibitor of prostaglandin synthesis) is used to ↓ t°.
3) cause
pulsating headache, which may be revealed in 20 minutes by the administration
of aspirin;
4) ↓
BP, therefore they are used in treatment of hypertension;
5) dilate
bronchi, therefore may be used in treatment of bronchial asthma;
6) ↓
secretion of HCl in the stomach, therefore are used in the therapy of ulcers
(aspirin and glucocorticoids ↓ synthesis of prostaglandins which ↓ HCl
secretion; therefore the improper use of aspirin or the prolonged therapy with
glucocorticoids may lead to ulcers in the stomach);
Prostaglandins F:
-
stimulate peristalsis of the bowel;
-
constrict bronchi;
-
stimulate the smooth muscle of the uterus,
therefore they are used for infant delivery.
7. Disorders of functions of endocrine glands: hyper-
and hypoproduction of hormones.




Comments
Post a Comment