BIOCHEMISTRY OF VITAMINS.
CLASS № 31
THEME:
BIOCHEMISTRY OF NUTRITION. VITAMINS THEORETICAL PART
1.
Components of human food. The significance of nutrition for the vital activity.
Essential food components. Causes and biochemical characteristics of
malnutrition syndrome
2.
Pathological states related to nutrition disorders: protein-energy malnutrition
– kwashiorkor, marasmus; causes and disturbance of metabolism.
3. Vitamins,
general characteristics, classification, biological functions. Vitaminlike
substances.
4. Sources
of vitamins for a human. Causes of hypo- and hypervitaminoses. Role of microflora
of large intestine in synthesis of some vitamins.
5.
Fat-soluble vitamins: A, D, E, and K, biological role, daily requirements,
dietary sources, symptoms of deficiency. Hypervitaminosis of some vitamins.
6.
Water-soluble vitamins: В1, В2, В6, В12, РР, С, pantothenic acid, biotin, folic
acid, biological role, daily requirements, dietary sources, symptoms of
deficiency.
7. The use
of vitamins in clinical practice. Polyvitamin medications.
8.
Anti-vitamins, mechanism of action, representatives, their application in
medical practice and scientific investigations.
Formulas for
memorizing: structure of vitamins A, D, В1, В2, В6, РР, С, and pantothenic
acid.
1. Components of human food. The
significance of nutrition for the vital activity. Essential food components.
Causes and biochemical characteristics of malnutrition syndrome
Nutritiology
(From the
greek “nutricia” food) - science about foods, nutrients and other components in
food, their interactions and role in maintaining health or disease, the
processes of consumption, uptake, transport, utilization(spending) and excretion.
CLASSIFICATION OF FOODS
●
Classification by origin:
-
Foods
of animal origin
-
Foods
of vegetable origin
●
Classification by chemical composition:
-
Fats
-
Proteins
-
Carbohydrates
-
Vitamins
-
Minerals
Main principles of nutrition
1. Caloric
intake should provide the body energy costs, which depend on age,
gender, type of physical or mental activity (for students of 2200-3000
kcal/day).
2. Rational
ratio of proteins, fats and carbohydrates, which for the average person is 1:1,5:4.
Most of the food carbohydrates constitute mainly of plant origin.
Usual daily
ration comprises 400-500 g carbohydrates
-
60-80%
are polysaccharides (mainly starch, a lesser amount glycogen and fiber
–cellulose)
-
20-30%
of oligosaccharides (sucrose, lactose, maltose)
-
the
rest quantity - monosaccharides (glucose, fructose and pentose).
Approximately
equal ratios of dietary fat (100 g/day) should be present saturated,
monounsaturated and polyunsaturated fatty acids.
Normal
nutritional amount of protein from 80 to 100 g/day, and it should be
ensured as proteins of plant origin and animal (in equal parts).
3. Food
essential components, many of which are present in minimal quantities (minor substances)
essential amino acids, essential fatty acids (linoleic, linolenic,
arachidonic), vitamins, minerals, fiber, components, essential oils, as well as
water.
4. Mode
of eating, which includes the multiplicity of reception and distribution of
the daily diet, morning – dinner – evening.
5. Match
diet physiological (or pathological) status of the organism (restriction of
carbohydrates in diabetes, proteins - with renal disease, lipids – in
atherosclerosis).
6. Food must
be subjected to cooking to increase the organoleptic properties and safety to
the organism.
General characteristics of the main components of food
01. PROTEINS
● Proteins
are complex organic nitrogenous compounds.
● They also
contain sulfur and, in some cases, phosphorous and iron.
● Proteins
are made of monomers called amino acids.
● There are
about 20 different amino acids which found in human body.
● Of these 8
amino acids are termed “essential” as
they are not
synthesized in human body and must be obtained from dietary proteins.
Functions
of Proteins
● Body
building
● Repair and
maintenance of body tissues
●
Maintenance of osmotic pressure
● Synthesis
of bioactive substances and other vital molecules
Assessment
of Protein nutrition status
● Protein
nutrition status is measured by Serum Albumin Concentration.
● It should
be more than 35 g/l.
-
Less
than 35 g/l shows mild malnutrition.
-
Less
than 30 g/l shows severe malnutrition.
02. FAT
Most of the
body fat (99 per cent) in the adipose tissue is in the form of triglyceroles,
in normal human subjects, adipose tissue constitutes between 10 and 15 per cent
of body weight.
One kilogram
of adipose tissue corresponds to 7700 kcal of energy.
Essential
fatty acids are those that cannot be synthesized by humans
Dietary
sources of Essential fatty acids
● Linoleic
acid- Sunflower oil Corn oil Soya bean oil Sesame oil Groundnut oil Mustard oil
Palm oil Coconut oil
●
Arachidonic acid - Meat, eggs, milk
● Linolenic
acid - Soya bean oil, Leafy greens
Functions
of fats
● They are
high energy foods, providing as much as 9 kcal for every gram.
● Fats serve
as vehicles for fat-soluble vitamins
● Fats in
the body support viscera such as heart, kidney and intestine; and fat beneath
the skin provides insulation against cold.
The
“non-calorie” roles of fat
● vegetable
fats are rich sources of essential fatty acids which are needed by the body for
growth, structural integrity of the cell membrane and decreased platelet
adhesiveness.
● Diets rich
in essential fatty acids have been reported to reduce serum cholesterol and low
density lipoproteins.
●
Polyunsaturated fatty acids are precursors of prostaglandins.
03. CARBOHYDRATE
Carbohydrate
is the main source of energy, providing 4 Kcals per one gram.
Carbohydrate
is also essential for the oxidation of fats and for the synthesis of certain
non-essential amino acids.
Sources
of carbohydrates
There are three main sources of carbohydrate, are starches, sugar and cellulose.
This reserve
is rapidly exhausted when a man is fasting. If the dietary carbohydrates do not
meet the energy needs of the body, protein and glycerol from dietary and
endogenous sources are used by the body to maintain glucose homeostasis.
04. Dietary fibre
Dietary
fibre which is mainly non-starch polysaccharide is a physiological important
component of the diet.
It is found
in vegetables, fruits and grains.
It may be
divided broadly into cellulose and noncellulose polysaccharides which include
hemicellulose pectin, storage polysaccharides like inulin, and the plant gums
and mucilage.
These are
all degraded to a greater of lesser extend by the micro flora in the human
colon.
MALNUTRITION
●
Malnutrition essentially means “bad nourishment”.
It concerns not
enough as well as too much food, the
wrong types of food, or the inability to use nutrients properly
to maintain health.
● The World
Health Organization cites malnutrition as the greatest single threat to
the world's public health.
●
Malnutrition in all its forms is a considerable public health concern
and is associated with increases risk of disease and early death.
● The World
Health Organization defines malnutrition as "the cellular imbalance
between supply of nutrients & energy and the body's demand for them to
ensure growth, maintenance, and specific functions”.
●
Malnutrition comprises both;
1. Under nutrition
2. Over nutrition
2. Pathological states related to
nutrition disorders: protein-energy malnutrition – kwashiorkor, marasmus;
causes and disturbance of metabolism.
TYPES OF
MALNUTRITION
01. Under nutrition is depletion of energy
(calories) resulting form insufficient food intake over an extended period
of time.
02. In extreme cases under-nutrition is called Starvation. While Famine is
severe food shortage of a whole community.
03. Specific Deficiency
is the pathological state resulting form a deficiency of an individual
nutrient such as vitamin A deficiency, iodine deficiency.
04. Over nutrition:
-
Many
tend to think malnutrition only in terms of hunger, however, overeating
is also a contributing factor.
-
“Over
nutrition is the pathological state resulting from the consumption of
excessive quantity of food over an extended period of time”.
-
Overweight and obesity are very common conditions in developed society and are becoming
more common in developing societies and those in transition.
NUTRITIONAL
DEFICIENCY DISEASES
On global
scale the five principal nutritional deficiency diseases are:
1.Kwashiorkor
2.Marasmus
3.Xerophthalmia
5.Endemic
goiter
MANIFESTATIONS
OF UNDER NUTRITION
● Under
nutrition results in the loss of body weight. The loss of weight is a
manifestation of energy depletion.
●
Malnutrition from any cause retards normal growth. Malnourished children
grow up with worse health and lower educational achievements.
● Decrease
in immunity increases the susceptibility to infections, which add to the morbidity
and mortality.
●
Malnutrition is also associated with lowered vitality of the people
leading to lowered productivity and reduced life expectancy.
MANIFESTATIONS
OF OVERNUTRITION
● In the
more developed countries of the world, over nutrition is encountered much more
frequently than under nutrition.
● The health
hazards from overnutrition are:
1. Obesity
2. Diabetes
3. Hypertension
4. cardiovascular diseases
5. renal diseases
6. Disorders of liver and gall bladder
3. Vitamins, general characteristics,
classification, biological functions. Vitaminlike substances.
Vitamins are
essential organic compounds that
-
the
body is not capable to synthesize (excl. D, PP)
-
required
in small amounts for maintaining metabolic integrity
•
Used
for synthesis of coenzymes and signaling substances or act as antioxidants.
•
are
neither plastic material nor energy source
Classification of vitamins
A character,
the chemical name and the name of the pathology to be treated
01. Fat-soluble vitamins:
1. A, retinol (antixerofthalmic).
2. D; calciferol (antiricketic).
3. E, tocopherols (antisteril, vitamin
of fertility).
4. K; naphthoquinones
(antihaemorrhagic).
02. Water-soluble vitamins:
1. B1, thiamine (antinevritic).
2. B2, riboflavin (vitamin of growth).
3. B3, pantothenic acid (antidermatic).
4. B6, pyridoxine (antidermatic).
5. B12, cyanocobalamin (antianemic).
6. PP, nicotinamide, nicotinic acid,
niacin (antipellagric).
7. Bc, folic acid (antianemic).
8. H, biotin (anti-seborrhoeic).
9. C, ascorbic acid (antiscurvic).
10.P, rutin.
•
Requirements
– from micrograms to tens
of milligrams per day.
– are influenced by age,
sex, and physiological conditions (pregnancy, breast-feeding, physical
exercise, and nutrition).
•
only
a few vitamins can be stored (A, D, E,
B12)
– lack of vitamins
quickly leads to deficiency diseases (hypovitaminoses)
•
hypervitaminoses (effects of overdose) with toxic symptoms
-
known
for vitamins A and D only.
- Normally, excess vitamins are rapidly excreted
Vitamin-like compounds
group of
substances, partly synthesized in the body, but possess some
properties of vitamins
No specific
clinical symptoms of deficiency
• B4,
choline (lipotropic factor).
• B8,
inositol (lipotropic factor).
• B13,
orotic acid (growth factor).
• B15,
pangamic acid.
• Bt,
carnitine.
• N, lipoic
acid.
• U
(anti-ulcer).
• PABA,
para-aminobenzoic acid.
• F
(linoleic, linolenic and arachidonic acid).
• Coenzyme
Q.
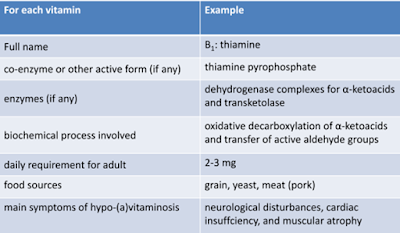
General plan of answer Example
• For
self-study:
– History of
discovery and investigations of vitamins
– causes of
deficiency of vitamins
Classification of vitamins according to their biochemical function
01. coenzyme
vitamins (B1, B2, B6, B12, PP, K, folic acid, biotin, etc.);
02. precursors
of signal molecules, with active forms
–
having
hormonal activity (D)
–
regulating
protein synthesis/gene expression (A, active form - retinoic acid, plays
role in growth and differentiation of cells) ;
03. antioxidant
vitamins (E, carotenes, bioflavonoids).
04. multifunctional
action (C: antioxidant and coenzyme).
Metabolism of vitamins
vitamins cannot
function in the form in which they are supplied with food.
Stages of
vitamins metabolism:
1. absorption in the intestine with special
transport systems;
2. transport to target organ/tissue of action/depot
via transport proteins;
3. conversion
(biotransformation) to active
(coenzyme) form using special enzyme systems;
4. proteidization with corresponding apo-enzyme
4. Sources of vitamins for a human.
Causes of hypo- and hypervitaminoses. Role of microflora of large intestine in
synthesis of some vitamins.
The source
of vitamins for humans is food.
An important
role in the formation of vitamins belongs to intestinal bacteria that
synthesize a number of vitamins.
Water-soluble
vitamins are not
accumulated in tissues (except vitamin B12), and therefore must be ingested
daily.
Fat-soluble
vitamins can accumulate
in tissues.
Their
deficiency is less common.
Imbalance of
vitamins in the body can be caused by their shortage as well as excess.
Shortage
in vitamins intake
with food causes a disease called hypovitaminosis.
In the complete absence of food avitaminosis (complete vitamin deficiency disease) develops.
It is
characteristic of fat-soluble vitamins.
Some
vitamins enter the body with food in the form of inactive precursors –
provitamins which tissues are converted into biologically active forms of
vitamins.
Hypovitaminosis
The human
need for vitamins depends on gender, age, physiological condition and the
intensity of labor.
The climatic
conditions and a nature of food have significant impact on an individual's need
for vitamins (the predominance of carbohydrate or protein in the diet, the
quantity and quality of fat).
In clinical
practice, the most frequent is hypovitaminosis.
Vitamin
deficiencies can be hidden or pronounced, appearing in relevant diseases.
Inadequate
intake of vitamins negatively affects
-
the
growth and development of children,
-
reduces
endurance,
-
physical
and mental performance,
-
increases
the impact of unfavorable environmental factors.
Vitamin
deficiency reduces the activity of the immune system, accelerates the aging
process.
The main
causes of hypovitaminosis are
1. lack of vitamins with food
2. malabsorption in the digestive tract
3. decay of vitamins in the gut
microflora due to its development
4. increased need for vitamins (stress,
physical activity, smoking, alcohol)
5. congenital defects in the enzymes
involved in the conversion into vitamin coenzymes
6. effects of structural analogues of
vitamins (antivitamin).
Hypervitaminosis
Diseases
arising from excessive intake of soluble vitamins have not been described.
Hypervitaminosis
is manifested in common symptoms:
-
loss
of appetite,
-
disorder
of motor function of the gastrointestinal tract,
-
headaches,
-
hair
loss,
-
peeling
skin,
-
increased
excitability of the nervous system and some specific features inherent in this
vitamin.
Hypervitaminosis
can be fatal.
5. Fat-soluble vitamins: A, D, E, and
K, biological role, daily requirements, dietary sources, symptoms of
deficiency. Hypervitaminosis of some vitamins
Lipid-soluble
vitamins
• vitamins
A, D, E, and K
• can be
absorbed efficiently only when there is normal fat absorption.
•
transported in the blood in lipoproteins or attached to specific
binding proteins
• belong to
the isoprenoids
Vitamin A
• Retinol,
presents in meat (as ester),
• provitamin
(β-carotene), found in plants
• converted
to retinaldehyde by dioxygenase
– (6 mg into
1 mg of retinol)
• Active forms:
o
retinaldehyde
utilized in vision
o
retinoic
acid acts in the control of gene expression, cell differentiation
• Deficiency: night blindness, xerophthalmia
• Through retinoid
X receptors: impairs functions of D and thyroid hormones

Daily
requirement in retinol activity equivalent (RAE)
900 – 3000
μg RAE/day for men
700 – 3000
μg RAE/day for women
1 μg RAE =
corresponds to
-
1
μg retinol,
-
2
μg of β-carotene in oil,
-
12
μg of "dietary" beta-carotene
Vitamin D
• precursor of the hormone calcitriol (1α,25-dihydroxycholecalciferol)
in lever and kidney
• regulates the Ca and P homeostasis
•
Synthesized in the skin from 7dehydrocholesterol, by a photochemical
reaction
• Vitamin D-binding
globulin – storage form
deficiencies only
occur when
-
the
skin receives insufficient UV light
-
and
vitamin D is lacking in the diet
rickets in children, osteomalacia in
adults (bone mineralization is disturbed)
High doses: Can reduce risk of diabetes, metabolic syndrome, cancer (prostate,
colorectal)
Vitamin E (tocopherols, tocotrienols)
• occurs only in plants
• located in
the membranes and plasma
• antioxidant,
chain-braking anti-radical
• protects unsaturated
lipids against free radicals
• tocopheroxyl
radical is reduced back to tocopherol by reaction with vitamin C
• 10 mg/day
for adults
• Deficiency: caused by abnormalities in
dietary fat absorption, not dietary
–
Neuromuscular and neurological problems
–
Hemolytic anemia
–
due
to oxidative damage to red blood cells
–
Retinopathy
–
Impairment
of the immune response
Vitamin K (K1: phylloquinone, K2: metaquinone)
• K1 is made by plants, found
in highest amounts in green leafy vegetables
• Animals may also convert K1 to K2
• Bacteria: K1 and K2
• carboxylating
Glu residues of blood coagulation factors VII, IX, X, proteins C and S in
the liver (cofactor of gamma-glutamyl carboxylase)
• Reduction
to coenzyme is inhibited by coumarins (prevent reduction of vit. K epoxide)
•
Requirement: 70 μg/day
• Deficiency: bleeding
6. Water-soluble vitamins: В1, В2, В6, В12, РР, С, pantothenic acid, biotin, folic acid, biological role, daily requirements, dietary sources, symptoms of deficiency.
B1 (Thiamin)
• Key role
in carbohydrate metabolism
i. Thiamine diphosphate - TPP (coenzyme)
ii. Thiamine triphosphate (neuroactive
form, Cl- channels in neurons)
• TPP is
a coenzyme of
–
pyruvate
dehydrogenase and 2-oxoglutarate dehydrogenase and
–
branched-chain
α-keto acid dehydrogenase
–
oxidative
decarboxylation and conjugation with coenzyme A
–
Transketolase
- transfer of two-carbon units
–
pyruvate
decarboxylase (in yeast)
• Food sources: whole grains, legumes, and some
meats and fish.
• Dietary requirement: 1.2 mg/day
• Deficiency: beriberi and Wernicke
encephalopathy.
B2 (Riboflavin)
• Coenzyme forms: Flavin mononucleotide (FMN),
flavin adenine dinucleotide (FAD)
• In ETC: FMN in Complex I and FAD in Complex II
• FAD is
required for the production of pyridoxic acid from pyridoxal
(vitamin B6) by pyridoxine 5'-phosphate oxidase
• Oxidative
decarboxylation of pyruvate, α-ketoglutarate requires FAD in the E3 portion of
their dehydrogenase complexes
• Fatty acyl
CoA dehydrogenase requires FAD in fatty acid β-oxidation
• FAD is required
to convert retinol to retinoic acid via cytosolic retinal dehydrogenase
• Synthesis
of an active form of folate (5-methyl-TH4) from 5,10-methylene-TH4 by
methylenetetrahydrofolate reductase is FADH2 dependent
• FAD is
required by kynurenine 3-monooxygenase to convert tryptophan to niacin
(vitamin PP)
Dietary requirement: 1.8 mg/day for women and 2.5 mg/day for men
Deficiency: angular stomatitis, cheilosis, anemia (interference with iron
absorption), in pregnancy - birth defects (congenital heart defects, limb
deformities)
Vitamin C
• Food source: citrus fruits, kiwifruit, guava, broccoli, Brussels sprouts, bell peppers and strawberries.
Prolonged
storage or cooking may reduce vitamin C content.
Human lacks
the L-Gulono-γ-lactone oxidase so unable to synthesize vitamin C.
• Daily requirements: 75-90 mg/day
• Deficiency: scurvy.
• C -
water-soluble antioxidant, maintains vitamin E and many metal cofactors in the
reduced state and has specific roles in the
– copper-containing
hydroxylases (synthesis of catecholamines)
–
iron-containing hydroxylases (proline and lysine hydroxylases)
–
modification of procollagen, blood clotting, synthesis of carnitine
Vitamin C is
a powerful reducing agent capable of rapidly scavenging a number of
reactive oxygen species (ROS).
Vitamin C functions as a cofactor for enzymes:
• Three
groups of enzymes (prolyl-3-hydroxylases, prolyl-4-hydroxylases, and lysyl
hydroxylases) that are required for the hydroxylation of proline and lysine in
the synthesis of collagen.
Hydroxylation
allows the collagen molecule to assume its triple helix structure, and thus
vitamin C is essential to the development and maintenance of scar tissue, blood
vessels, and cartilage.
The role of
vitamin C is to oxidize prolyl hydroxylase and lysyl hydroxylase from
Fe2+ to Fe3+ and to reduce it from Fe3+ to Fe2+.
• Two enzymes (ε-N-trimethyl-L-lysine
hydroxylase and γ-butyrobetaine hydroxylase) of synthesis of carnitine.
• Hypoxia-inducible factor-proline dioxygenase
enzymes
• synthesis
and catabolism of tyrosine
• Dopamine beta-hydroxylase - biosynthesis of norepinephrine from dopamine
Niacin (PP)
• Can be synthesized
by plants and animals from tryptophan.
• highest
contents in meat, poultry, red fish (tuna and salmon), lesser amounts in
nuts, legumes and seeds.
• Coenzyme form: Nicotinamide is a component of
the coenzymes nicotinamide adenine dinucleotide (NAD+) and nicotinamide adenine
dinucleotide phosphate (NADP+)
Daily requirements: 14 mg/day for adult women, 16 mg/day for adult men
Deficiency: pellagra - can be caused by deficiency of both Tryptophan and niacin
or:
–
Hartnup
disease: defect in membrane transporter for tryptophan
–
Carcinoid
syndrome – overproduction of serotonin by liver tumor or enterochromaffin cells
(using up tryptophan)
Additional functions Water-soluble vitamins participate:
• B6 as
pyridoxal phosphate (PALP) is the coenzyme
–
in
amino acid metabolism, including the transaminases,
–
and
of glycogen phosphorylase
• Biotin
is the coenzyme for carboxylase enzymes and has a role in regulation of the
cell cycle (biotinylation of key nuclear proteins)
• B12 and
folic acid take part in providing one-carbon residues for DNA synthesis.
Conversion of CH3-FH4 to FH4 requires B12!
• PP:
NAD+ is a source of ADP-ribose for ADP-ribosylation of proteins and
polyADP-ribosylation of nucleoproteins in the DNA repair.
Water-soluble vitamins - deficiencies
PP
• Vitamin
deficiency only occurs when PP and tryptophan are simultaneously
lacking in
the diet
• 60 mg of
tryptophan in diet is equivalent to 1 mg of PP
Folate
• disturbances
in nucleotide biosynthesis and cell proliferation
•
deficiency: megaloblastic anemia, impaired phospholipid synthesis and amino
acid metabolism • Sign of deficiency – hyperhomocystienemia
B12
• Not in
plant products! (synthetized by flora)
• Deficiency
is due to an absence of intrinsic factor - resorption disturbance.
• Clinical
signs same as for folate deficiency
C
• Sign of
deficiency – methylmalonic aciduria Iron- (Pro, Lys, Asp) and copper-
(dopamine, peptidylglycine) containing hydroxylases
• deficiency:
skin changes, fragility of blood capillaries, gum decay, tooth loss, and bone
fracture attributed to deficient collagen synthesis
• increased
intakes may be beneficial: enhances the absorption of iron
7. The use of vitamins in clinical
practice. Polyvitamin medications.
Application
of vitamins in clinics
• Prevention
of hypovitaminosis due to
–
low
intake of vitamins from food
–
Increased
vitamin requirements (stress, exposure to harmful environmental factors,
pregnancy)
• reducing
the risk of colds, cardiovascular, cancer and other diseases
• Treatment
of primary (food) vitamin deficiencies
• Treatment
of metabolic disorders (incl. congenital) and secondary vitamin
deficiencies due to:
-
pathological
processes
-
surgeries
-
drug
therapy
-
dietary
restrictions
• The use
vitamins in high doses for treatment of diseases
High doses of vitamins
• Vitamin A - prevention of infertility,
increased tissue regeneration, to stimulate the growth and development of
children.
• Vitamin C – enhances absorption of inorganic
ions (Fe)
• Vitamin D -
rickets and treatment of skin diseases, prevention of colon cancer.
• Vitamin K - for bleeding associated with a
decrease in blood clotting.
• Vitamin E – protection of pregnancy and
threatened abortion, liver disease, muscle atrophy, congenital disorders of
erythrocyte membranes in the newborn.
• Vitamin B1 -
diabetes mellitus (to improve digestion of carbohydrates), inflammation of the
peripheral nerves and lesions of the nervous system, heart and muscles.
• Vitamin B2 -
dermatitis, poorly healing wounds and ulcers, keratitis, conjunctivitis, liver
damage.
• Pantothenic acid -
skin and hair diseases, hepatitis, myocardium dystrophy.
• Vitamin PP - dermatitis,
lesions of peripheral nerves, myocardium dystrophy.
• Vitamin B6 - polyneuritis, dermatitis, toxemia
of pregnancy, hepatitis.
Intervitamin relationships
• C and E –
in trapping free radicals
• B12 and
folic acid – in DNA synthesis
• A and D in
Ca2+ homeostasis
Assessing the vitamin status
• direct
monitoring in biological fluids
• B6 – PALP
effect in vitro on erythrocyte transaminases
• B1 – TDP
effect
• C -
excretion after loading
• by level
of metabolites in blood/urine (for folate - homocysteine, for B1 - pyruvate)
8. Anti-vitamins, mechanism of action,
representatives, their application in medical practice and scientific
investigations.
Antivitamins
substances causing
reduction or complete loss of biological activity of vitamins by:
• destruction
of vitamin or its binding molecule to inactive forms
–
egg
white protein avidin forms insoluble complex with biotin and prevents biotin
absorption in intestine
–
thiaminase
destroys thiamine (B1)
–
lipooxydase
oxidates carotene
• replacing
coenzyme in the active sites of enzyme (structural analogs of vitamins or
coenzymes)
–
sulfonamines
(structural analogs of PABA)
–
coumarins
(antivitamins K)
–
hydrazide
of isonicotinic acid (antivitamin PP)














Comments
Post a Comment